Special report: Bone Densitometry market on the mend
May 09, 2011
This report originally appeared in the May 2011 issue of DOTmed Business News
By Kathy F. Mahdoubi, DOTmed News
Only a few years ago, the bone densitometry industry was in bad shape. Doctors faced steep Medicare reimbursement cuts and patients had limited access to bone-density tests. But now, the market might be bouncing back with increased reimbursement and recommendations that expand the patient population for osteoporosis screening.
Fortifying CMS reimbursement
Those outside the industry may be surprised to learn that the total annual cost of fall injuries is expected to swell to almost $60 billion by 2020, according to the Centers for Disease Control and Prevention. That statistic is in contrast to a history of conservative Medicare reimbursement for bone mineral density testing, otherwise known as dual-energy X-ray absorptiometry (DXA). The cuts in question began rolling out as a part of the CMS Physician Fee Schedule just four years ago. A test in a non-hospital setting that might have been reimbursed at $140 in 2006 has seen that amount dwindle down to about $40 in 2010.
These dismal numbers have been adjusted thanks to a two-year reprieve by Congress as a part of the Affordable Care Act signed into law last year. To physicians’ relief, Medicare reimbursement is now back up to about $100 per study and has been made retroactive for claims filed in 2010.
Assumptions about utilization
What caused the drastic cuts were concerns over the explosive growth of DXA scans, according to Dr. Andrew Laster, immediate past president of the International Society for Clinical Densitometry and a working physician for Arthritis and Osteoporosis Consultants of the Carolinas based in Charlotte, N.C.
“CMS reviews those fees every five years and they identified on the last review a significant increase in the number of DXA claims they were receiving,” says Laster. “When they compared 1994 to 2004 they saw an increase from about 75,000 studies to roughly 2.5 million, both hospital and non-hospital.”
In recent years, Medicare has cracked down on what the agency deemed as misuse or overuse of complex imaging services, including CT and MRI scans, by slashing reimbursement for those procedures.
“Even though the number of DXA studies appears to have increased, it still represents a small fraction of the people that need to be tested,” says Laster. “When one looks at the numbers, about 13.3 percent of eligible Medicare beneficiaries have had a DXA study done in one year. This was not an issue of overuse, but growth promoted in part by the government.”
Government promotion of bone density testing has been gaining strength as a result of U.S. Food and Drug Administration-approved drug treatments for osteoporosis and recommendations by the surgeon general.
More recently, the U.S. Preventative Services Task Force has called to expand the population of screened women by recommending the screening of high-risk women under 65 – those who have as high a risk of fracture as women 65 and
older.
New recommendations for women under 65
According to a January release from the USPSTF, approximately 12 million Americans 50 years and older are expected to have osteoporosis by 2012. In addition, one-half of all postmenopausal women are expected to suffer an osteoporosis-related fracture during their lifetime.
Postmenopausal women under the age of 65 may be in just as much danger of a fracture if they are low on the body-mass index, smoke, have a high-alcohol intake or have a family history of fracture. Physicians now have a series of tools to calculate fracture risk, including FRAX, an algorithm developed by the World Health Organization that can predict a patient’s potential risk of fracture.
Dr. Ethel Siris, the immediate past president of the National Osteoporosis Foundation and director of the Toni Stabile Osteoporosis Center at Columbia University Medical Center in New York, is encouraged by the new recommendations for osteoporosis screening for at-risk women between 50 to 65 years of age.
“Their statement clearly legitimizes, with public health policy, the value of doing bone density testing in women who are at risk of fractures, whether it’s 65 and up or younger than 65 with risk factors,” says Siris. “One great value is that there is scientific review involved, which makes a more solid public health recommendation.”
Patient access further threatened
After Medicare reimbursement in the non-hospital setting was reduced, physician and patient advocacy groups including the ISCD and NOF rallied to reinstate a higher reimbursement rate.
“The issue of reimbursement is a serious one when juxtaposed with America’s poor access to bone density testing,” says Siris. “A new bone densitometer might cost a private or group practice $125,000, and at the height of CMS’s reimbursement lows, the reimbursements were not even covering the cost of the equipment.”
Practices that weren’t reimbursed at a level that covered their operating cost have phased-out their DXA services, discontinued their system contracts and laid off their X-ray techs, all of which has put manufacturers on the alert.
Impact on DXA sales
Laura Stoltenberg, general manager of the Lunar division of GE Healthcare, has seen signs of a downward trend for some physician practices.
“We have talked with various clinical groups and the concern with any changes in guidelines and reimbursement rates and the potential impact on what that does to clinical access to the equipment,” says Stoltenberg.
The impact of reimbursement cuts, according to Stoltenberg, had been an overall decline in the purchases or even a decrease in the return of leased equipment.
John Jenkins, vice president and general manager of skeletal health for Hologic, has also seen DXA sales from physician practices slow down, but says there was a time when physicians sought to provide more on-site services.
“Physicians were very interested in providing point-of-care assessment for osteoporosis, but what happened was that we saw our physician sales decline and our hospital sales actually get reinvigorated, because most of the systems at the hospital were end-of-life systems that were nearly 10 years old.”
Curtailed rural access
With services being cut back in private and group physician practices, more business is going to hospitals, which have not suffered the same reimbursement cuts as non-hospital settings. The increased business for hospitals is great news, except when you factor in the loss of local access for osteoporosis patients living in rural areas.
“Studies have shown that if patients have a drive of more than five to 10 miles from services, those services may not get [used],” says Laster. “Given the setting, where already an inadequate number of people are getting tested, if you restrict it further and make access less available, then you’ll have a hard time meeting the goals to increase screening to identify people at risk.”
Will new recommendations be enough?
The two-year lift on Medicare cuts for bone density testing will be reviewed again and further legislation will have to be enacted to continue the current level of reimbursement.
“If there isn’t further relief with new legislation, then the reimbursement would drop again to $47 in 2012 and $42 in 2013 in the non-hospital setting,” says Laster.
Even if new legislation keeps a larger slice of reimbursement, Siris says there are still glitches in filing Medicare claims. Physicians currently have approval to screen at-risk women at two-year intervals, but there is some difficulty getting the tests reimbursed. Medicare claims do get paid, but physicians have to jump through hoops.
“The rules of the CMS are that if you are being monitored for an FDA-approved treatment for osteoporosis, you can have a repeat test in less than 23 months after the first test in order to monitor people,” says Siris. “But whenever we do a one-year follow up during treatment inevitably [the claim] is rejected by the local Medicare carrier, even though we put the proper code in to indicate that is what we’re doing, and we have to go back and give them a lot more information.”
The problem of awareness
Siris states that many physicians do not heed patients’ need for osteoporosis testing and treatment in the same way they monitor risk and treat for heart attack and serious forms of cancer.
“The greatest challenge is still an awareness issue and this is a problem for patients and physicians alike,” says Siris. “People do not appreciate the seriousness of later-life fractures, which not only cost a lot of money to fix and have a significant impact on quality of life, but in the case of hip fracture, it has been associated with higher mortality.”
In fact, there is about a 20 percent increased risk of mortality for osteoporotic patients who have suffered a hip fracture, and statistics from the USPSTF note that more than one-third of men who have suffered a hip facture die within a year.
“This is something not to be taken lightly,” says Siris.
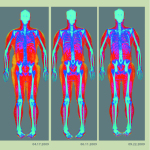
OEMs move to diversify
Both GE Healthcare and Hologic are offering skeletal health systems besides traditional bone densitometers. Their focus is expanding skeletal health to include the greater role of total body composition in disease risk and prevention.
GE’s bone densitometer brand, Lunar, includes the DPX and iDXA series of bone densitometry systems, as well as the Achilles quantitative ultrasound technology, which assesses the risk of fracture with a lightweight, portable device. Ultrasound is currently not used to diagnose osteoporosis or monitor treatment, but it is considered a complementary tool for predicting fracture risk.
“Some advancements in the technology along with the thinking, are really going beyond just looking at bone,” says Stoltenberg. “If you take a look at fracture risk or overall health of an individual, how much lean mass and fat you have is in a lot of cases as important as your bone strength. Having the appropriate amount of lean mass helps with stability and fracture prevention.”
GE also offers an over-the-counter device called InBody, which utilizes bioimpedence technology and sends a harmless electrical pulse through the body to quantify body composition. The manufacturer currently has pilot programs in assisted living facilities where advocacy groups help educate residents about how they can build muscle and reduce risk of fracture.
“We have a number of units already engaged with Brookdale, which is the largest national chain for assisted living facilities,” says Stoltenberg.
Back to DXA access
Sales of bone densitometry systems and patient access to services in private and group physicians’ offices may have declined, but they were by no means stifled completely during Medicare’s slump in reimbursement rates. Larger practices continued to buy DXA units. Manufacturers are also aware of the impact a flat or down-market has on patient access to screening.
“We’ll see additional growth in the traditional osteoporosis testing market if the reimbursement is locked in, if not, we’ll probably see growth remain stable. In the meantime, we are looking at additional clinical capabilities, which allow us to expand outside the traditional DXA markets,” says Jenkins.
Case in point, Hologic has been working to promote a new DXA procedure that can actually alert clinicians to cardiovascular disease by screening for abdominal aortic calcification.
“If you have calcium in your aorta, that is basically a risk factor for cardiovascular disease,” says Jenkins. “It correlates very strongly with calcification in your coronary arteries.”
Markers for growth
In order to really make a difference and improve access to bone density screening, Siris says it is the primary care doctors that need to be made aware of their role in osteoporosis prevention.
“Most people in America get their care from primary care doctors. We’ve got to get the primary care doctors aboard. Until we do, there is not going to be a lower risk of fractures.”
One major advance in the industry that may hold the ticket to better access for patients is the positive health data coming out of government-funded economic models. Data procured for U.S. Congress to assess the economic cost of fractures that occur every year show that there are very real benefits from screening large numbers of people. Some data suggest that large-scale screening could even lead to savings of more than $1 billion within five years, says Laster.
Ultimately, only time will tell if new health data, sufficient Medicare reimbursement and the adoption of expanded osteoporosis screening recommendations will be enough to patch the problem of patient access to osteoporosis screening in America.
DOTmed Registered Bone Densitometers Sales & Service Companies
Names in boldface are Premium Listings.
Domestic
Kevin McMahon, Unfors Instruments Inc, CT
Robert Serros, Amber Diagnostics, FL
DM 100
David Denholtz, BoneDensitometers.com, FL
DOTmed Certified
DM 100
Frank Pontillo, Ens, FL
Jeff Fisher, Fisher BioMedical, Inc., FL
Moshe Alkalay, Hi Tech Int'l Group, FL
DOTmed Certified
Ed Ruth, Managed Medical Imaging, FL
John Pereira, United Medical Technologies, FL
DM 100
John Jenkins, Hologic, MA
Davyn McGuire, Med Exchange International, Inc., MA
DOTmed Certified
DM 100
John Gladstein, Medical Device Depot, MD
DOTmed Certified
Becky Lowe, Block Imaging International, Inc., MI
DM 100
Tony Orlando, Complete Medical Services, MI
DOTmed Certified
DM 100
Alison Fortin, Global Inventory Management LLC, NH
DOTmed Certified
DM 100
Ryan Gilday, Clinical Imaging Systems, NJ
DM 100
Joseph Jenkins, International Imaging Ltd., NV
Abe Sokol, Absolute Medical Equipment, NY
DOTmed Certified
DM 100
Jeff Weiss, Atlantis Worldwide, LLC, NY
DM 100
John Kollegger, Bayshore Medical Equipment, Inc., NY
DOTmed Certified
DM 100
Ian Alpert, Tandem Medical Equipment, NY
DOTmed Certified
DM 100
William Jurgensen, First Choice Imaging, LLC, NY
Leon Gugel, Metropolis International, NY
DOTmed Certified
DM 100
Karlie Hartog, Med Tech Solutions, OK
Douglas Holmberg, DMS Imaging, SD
DM 100
Desmond Johnson, DEXAScanners, Inc., TN
Ben Williams, DEXA Solutions, LLC, WI
GE Healthcare Lunar, WI
International
David Lapenat, ANDA Medical, Inc., Canada
DOTmed Certified
DM 100
Efthimios Tentolouris, Tentolouris, Greece
Gautam Sehgal, Ads diagnostic limited, India
Kaushik Shah, K S BIOMED SERVICES, India
Eli Barkai, ElsMor Medical Systems Ltd, Israel
By Kathy F. Mahdoubi, DOTmed News
Only a few years ago, the bone densitometry industry was in bad shape. Doctors faced steep Medicare reimbursement cuts and patients had limited access to bone-density tests. But now, the market might be bouncing back with increased reimbursement and recommendations that expand the patient population for osteoporosis screening.
Fortifying CMS reimbursement
Those outside the industry may be surprised to learn that the total annual cost of fall injuries is expected to swell to almost $60 billion by 2020, according to the Centers for Disease Control and Prevention. That statistic is in contrast to a history of conservative Medicare reimbursement for bone mineral density testing, otherwise known as dual-energy X-ray absorptiometry (DXA). The cuts in question began rolling out as a part of the CMS Physician Fee Schedule just four years ago. A test in a non-hospital setting that might have been reimbursed at $140 in 2006 has seen that amount dwindle down to about $40 in 2010.
These dismal numbers have been adjusted thanks to a two-year reprieve by Congress as a part of the Affordable Care Act signed into law last year. To physicians’ relief, Medicare reimbursement is now back up to about $100 per study and has been made retroactive for claims filed in 2010.
Assumptions about utilization
What caused the drastic cuts were concerns over the explosive growth of DXA scans, according to Dr. Andrew Laster, immediate past president of the International Society for Clinical Densitometry and a working physician for Arthritis and Osteoporosis Consultants of the Carolinas based in Charlotte, N.C.
“CMS reviews those fees every five years and they identified on the last review a significant increase in the number of DXA claims they were receiving,” says Laster. “When they compared 1994 to 2004 they saw an increase from about 75,000 studies to roughly 2.5 million, both hospital and non-hospital.”
In recent years, Medicare has cracked down on what the agency deemed as misuse or overuse of complex imaging services, including CT and MRI scans, by slashing reimbursement for those procedures.
“Even though the number of DXA studies appears to have increased, it still represents a small fraction of the people that need to be tested,” says Laster. “When one looks at the numbers, about 13.3 percent of eligible Medicare beneficiaries have had a DXA study done in one year. This was not an issue of overuse, but growth promoted in part by the government.”
Government promotion of bone density testing has been gaining strength as a result of U.S. Food and Drug Administration-approved drug treatments for osteoporosis and recommendations by the surgeon general.
More recently, the U.S. Preventative Services Task Force has called to expand the population of screened women by recommending the screening of high-risk women under 65 – those who have as high a risk of fracture as women 65 and
older.
New recommendations for women under 65
According to a January release from the USPSTF, approximately 12 million Americans 50 years and older are expected to have osteoporosis by 2012. In addition, one-half of all postmenopausal women are expected to suffer an osteoporosis-related fracture during their lifetime.
Postmenopausal women under the age of 65 may be in just as much danger of a fracture if they are low on the body-mass index, smoke, have a high-alcohol intake or have a family history of fracture. Physicians now have a series of tools to calculate fracture risk, including FRAX, an algorithm developed by the World Health Organization that can predict a patient’s potential risk of fracture.
Dr. Ethel Siris, the immediate past president of the National Osteoporosis Foundation and director of the Toni Stabile Osteoporosis Center at Columbia University Medical Center in New York, is encouraged by the new recommendations for osteoporosis screening for at-risk women between 50 to 65 years of age.
“Their statement clearly legitimizes, with public health policy, the value of doing bone density testing in women who are at risk of fractures, whether it’s 65 and up or younger than 65 with risk factors,” says Siris. “One great value is that there is scientific review involved, which makes a more solid public health recommendation.”
Patient access further threatened
After Medicare reimbursement in the non-hospital setting was reduced, physician and patient advocacy groups including the ISCD and NOF rallied to reinstate a higher reimbursement rate.
“The issue of reimbursement is a serious one when juxtaposed with America’s poor access to bone density testing,” says Siris. “A new bone densitometer might cost a private or group practice $125,000, and at the height of CMS’s reimbursement lows, the reimbursements were not even covering the cost of the equipment.”
Practices that weren’t reimbursed at a level that covered their operating cost have phased-out their DXA services, discontinued their system contracts and laid off their X-ray techs, all of which has put manufacturers on the alert.
Impact on DXA sales
Laura Stoltenberg, general manager of the Lunar division of GE Healthcare, has seen signs of a downward trend for some physician practices.
“We have talked with various clinical groups and the concern with any changes in guidelines and reimbursement rates and the potential impact on what that does to clinical access to the equipment,” says Stoltenberg.
The impact of reimbursement cuts, according to Stoltenberg, had been an overall decline in the purchases or even a decrease in the return of leased equipment.
John Jenkins, vice president and general manager of skeletal health for Hologic, has also seen DXA sales from physician practices slow down, but says there was a time when physicians sought to provide more on-site services.
“Physicians were very interested in providing point-of-care assessment for osteoporosis, but what happened was that we saw our physician sales decline and our hospital sales actually get reinvigorated, because most of the systems at the hospital were end-of-life systems that were nearly 10 years old.”
Curtailed rural access
With services being cut back in private and group physician practices, more business is going to hospitals, which have not suffered the same reimbursement cuts as non-hospital settings. The increased business for hospitals is great news, except when you factor in the loss of local access for osteoporosis patients living in rural areas.
“Studies have shown that if patients have a drive of more than five to 10 miles from services, those services may not get [used],” says Laster. “Given the setting, where already an inadequate number of people are getting tested, if you restrict it further and make access less available, then you’ll have a hard time meeting the goals to increase screening to identify people at risk.”
Will new recommendations be enough?
The two-year lift on Medicare cuts for bone density testing will be reviewed again and further legislation will have to be enacted to continue the current level of reimbursement.
“If there isn’t further relief with new legislation, then the reimbursement would drop again to $47 in 2012 and $42 in 2013 in the non-hospital setting,” says Laster.
Even if new legislation keeps a larger slice of reimbursement, Siris says there are still glitches in filing Medicare claims. Physicians currently have approval to screen at-risk women at two-year intervals, but there is some difficulty getting the tests reimbursed. Medicare claims do get paid, but physicians have to jump through hoops.
“The rules of the CMS are that if you are being monitored for an FDA-approved treatment for osteoporosis, you can have a repeat test in less than 23 months after the first test in order to monitor people,” says Siris. “But whenever we do a one-year follow up during treatment inevitably [the claim] is rejected by the local Medicare carrier, even though we put the proper code in to indicate that is what we’re doing, and we have to go back and give them a lot more information.”
The problem of awareness
Siris states that many physicians do not heed patients’ need for osteoporosis testing and treatment in the same way they monitor risk and treat for heart attack and serious forms of cancer.
“The greatest challenge is still an awareness issue and this is a problem for patients and physicians alike,” says Siris. “People do not appreciate the seriousness of later-life fractures, which not only cost a lot of money to fix and have a significant impact on quality of life, but in the case of hip fracture, it has been associated with higher mortality.”
In fact, there is about a 20 percent increased risk of mortality for osteoporotic patients who have suffered a hip fracture, and statistics from the USPSTF note that more than one-third of men who have suffered a hip facture die within a year.
“This is something not to be taken lightly,” says Siris.
OEMs move to diversify
Both GE Healthcare and Hologic are offering skeletal health systems besides traditional bone densitometers. Their focus is expanding skeletal health to include the greater role of total body composition in disease risk and prevention.
GE’s bone densitometer brand, Lunar, includes the DPX and iDXA series of bone densitometry systems, as well as the Achilles quantitative ultrasound technology, which assesses the risk of fracture with a lightweight, portable device. Ultrasound is currently not used to diagnose osteoporosis or monitor treatment, but it is considered a complementary tool for predicting fracture risk.
“Some advancements in the technology along with the thinking, are really going beyond just looking at bone,” says Stoltenberg. “If you take a look at fracture risk or overall health of an individual, how much lean mass and fat you have is in a lot of cases as important as your bone strength. Having the appropriate amount of lean mass helps with stability and fracture prevention.”
GE also offers an over-the-counter device called InBody, which utilizes bioimpedence technology and sends a harmless electrical pulse through the body to quantify body composition. The manufacturer currently has pilot programs in assisted living facilities where advocacy groups help educate residents about how they can build muscle and reduce risk of fracture.
“We have a number of units already engaged with Brookdale, which is the largest national chain for assisted living facilities,” says Stoltenberg.
Back to DXA access
Sales of bone densitometry systems and patient access to services in private and group physicians’ offices may have declined, but they were by no means stifled completely during Medicare’s slump in reimbursement rates. Larger practices continued to buy DXA units. Manufacturers are also aware of the impact a flat or down-market has on patient access to screening.
“We’ll see additional growth in the traditional osteoporosis testing market if the reimbursement is locked in, if not, we’ll probably see growth remain stable. In the meantime, we are looking at additional clinical capabilities, which allow us to expand outside the traditional DXA markets,” says Jenkins.
Case in point, Hologic has been working to promote a new DXA procedure that can actually alert clinicians to cardiovascular disease by screening for abdominal aortic calcification.
“If you have calcium in your aorta, that is basically a risk factor for cardiovascular disease,” says Jenkins. “It correlates very strongly with calcification in your coronary arteries.”
Markers for growth
In order to really make a difference and improve access to bone density screening, Siris says it is the primary care doctors that need to be made aware of their role in osteoporosis prevention.
“Most people in America get their care from primary care doctors. We’ve got to get the primary care doctors aboard. Until we do, there is not going to be a lower risk of fractures.”
One major advance in the industry that may hold the ticket to better access for patients is the positive health data coming out of government-funded economic models. Data procured for U.S. Congress to assess the economic cost of fractures that occur every year show that there are very real benefits from screening large numbers of people. Some data suggest that large-scale screening could even lead to savings of more than $1 billion within five years, says Laster.
Ultimately, only time will tell if new health data, sufficient Medicare reimbursement and the adoption of expanded osteoporosis screening recommendations will be enough to patch the problem of patient access to osteoporosis screening in America.
DOTmed Registered Bone Densitometers Sales & Service Companies
Names in boldface are Premium Listings.
Domestic
Kevin McMahon, Unfors Instruments Inc, CT
Robert Serros, Amber Diagnostics, FL
DM 100
David Denholtz, BoneDensitometers.com, FL
DOTmed Certified
DM 100
Frank Pontillo, Ens, FL
Jeff Fisher, Fisher BioMedical, Inc., FL
Moshe Alkalay, Hi Tech Int'l Group, FL
DOTmed Certified
Ed Ruth, Managed Medical Imaging, FL
John Pereira, United Medical Technologies, FL
DM 100
John Jenkins, Hologic, MA
Davyn McGuire, Med Exchange International, Inc., MA
DOTmed Certified
DM 100
John Gladstein, Medical Device Depot, MD
DOTmed Certified
Becky Lowe, Block Imaging International, Inc., MI
DM 100
Tony Orlando, Complete Medical Services, MI
DOTmed Certified
DM 100
Alison Fortin, Global Inventory Management LLC, NH
DOTmed Certified
DM 100
Ryan Gilday, Clinical Imaging Systems, NJ
DM 100
Joseph Jenkins, International Imaging Ltd., NV
Abe Sokol, Absolute Medical Equipment, NY
DOTmed Certified
DM 100
Jeff Weiss, Atlantis Worldwide, LLC, NY
DM 100
John Kollegger, Bayshore Medical Equipment, Inc., NY
DOTmed Certified
DM 100
Ian Alpert, Tandem Medical Equipment, NY
DOTmed Certified
DM 100
William Jurgensen, First Choice Imaging, LLC, NY
Leon Gugel, Metropolis International, NY
DOTmed Certified
DM 100
Karlie Hartog, Med Tech Solutions, OK
Douglas Holmberg, DMS Imaging, SD
DM 100
Desmond Johnson, DEXAScanners, Inc., TN
Ben Williams, DEXA Solutions, LLC, WI
GE Healthcare Lunar, WI
International
David Lapenat, ANDA Medical, Inc., Canada
DOTmed Certified
DM 100
Efthimios Tentolouris, Tentolouris, Greece
Gautam Sehgal, Ads diagnostic limited, India
Kaushik Shah, K S BIOMED SERVICES, India
Eli Barkai, ElsMor Medical Systems Ltd, Israel