Experts see shift to tomo-only breast imaging
July 24, 2017
by Lisa Chamoff, Contributing Reporter
While digital 2-D mammography remains a necessary part of cancer screening for the vast majority of women, new technologies are emerging that may help clear the path for digital breast tomosynthesis, also known as 3-D mammography, to become the new gold standard.
Most facilities that screen with tomosynthesis also capture an image via 2-D mammography, in order to give radiologists a look at the entire breast, as well as the individual layers of the breast that tomosynthesis provides.
A few facilities have been studying a new technique that uses the data obtained during tomosynthesis imaging and compresses it to create a synthesized 2-D-like composite image. This, in turn, lowers the radiation dose, as a woman does not need a mammogram in addition to tomosynthesis, which exposes patients to more radiation than digital mammography.
In a study published last year in the journal Radiology, radiologists at the University of Pennsylvania compared recall rates, biopsy rates, cancer detection rates and radiation dose for more than 15,000 women screened with digital mammography and digital breast tomosynthesis between October 2011 and February 2013, as well as more than 5,000 women screened with digital breast tomosynthesis and synthesized 2-D mammography from January to June 2015.
The study found no significant difference in cancer detection rate for synthesized 2-D mammography and digital breast tomosynthesis versus digital mammography and tomosynthesis, while the average radiation dose was nearly 40 percent lower when the synthetic image was used.
The biopsy rate was also lower when synthesized 2-D mammography was used — 1.3 percent versus 2 percent for the digital mammography and tomosynthesis combination.
“We’ve shown it’s adequate,” says Emily Conant, chief of the division of breast imaging at the Hospital of the University of Pennsylvania and an author of the study. “It further reduces false positives and kept the cancer detection rate the same. If we can create a lower-dose, better mammogram, that’s better.”
Conant says that the 2-D picture is important for looking at a woman’s overall breast density and that some suspicious findings, such as calcium deposits, are more easily seen on a 2-D image. And while some radiologists don’t think the appearance of the synthetic image is as good as a standard 2-D mammogram image, Conant believes the synthesized 2-D mammography and tomosynthesis combination is the future of breast cancer screening.
“In the six years since we’ve implemented tomosynthesis in our clinics, we’ve really seen the impact that it makes,” Conant says. “This whole concept of synthetic imaging is the new kid on the block and it continues to improve. It’s evolving so rapidly. It can only get better.”
Digital breast tomosynthesis scanners from Hologic, GE Healthcare and Siemens Healthineers are all capable of providing the synthesized 2-D image.
Other clinicians have similarly shown that the synthesized 2-D image is adequate.
For a study published in the journal Radiology in February, researchers at the Christiana Care Health System’s Helen F. Graham Cancer Center & Research Institute looked at more than 32,000 women screened with just mammography, more than 30,000 screened with a combination of tomosynthesis and mammography and more than 16,000 women screened using the synthesized 2-D mammography over five years, a much larger sample size than previous studies.
The recall rate for synthesized 2-D mammography was 4.3 percent, compared to 5.8 percent for tomosynthesis and mammography and 8.7 percent for the 2-D mammography alone. More than 76 percent of invasive cancers were detected using synthesized 2-D mammography, versus more than 61 percent for tomosynthesis and mammography.
Using the synthesized 2-D mammography also decreased the radiation dose between 40 and 45 percent, says Dr. Jacqueline S. Holt, director of breast imaging at the Christiana Care Health System’s Helen F. Graham Cancer Center & Research Institute.
“I was hoping that this article showing performance in a real-world setting would tilt the dials,” Holt says. “The dose is down to where digital [mammography] was, plus we have the benefit of the 3-D images, plus we have the 2-D image. I think that this will be the new normal mammogram.”
Debra Monticciolo, chair of the American College of Radiology’s Commission on Breast Imaging, says that while preliminary results have shown that the synthesized 2-D image is equally diagnostic, she looks forward to the results of more studies on its use.
“We still do the standard digital mammography and add tomosynthesis to it,” says Monticciolo, who is also vice chair for research and section chief of breast imaging in the department of radiology at Baylor Scott & White Healthcare in Temple, Texas. “That’s the way we started and there wasn’t enough data yet to go with the composite. The composite has a different look than the standard 2-D image, which breast imagers will likely get used to over time.”
But even Monticciolo believes it will be a more common practice to use the synthesized image in the future.
“Over time, companies work on algorithms,” Monticciolo says. “Over time it will also improve.”
Hologic's C-View software, allowing radiologists to generate a 2-D image from the tomosynthesis dataset, has been available since February 2011.
“We've seen an increase in adoption rates as more and more clinical research is released demonstrating comparable invasive cancer detection rates and recall rates to traditional breast tomosynthesis screening exams,” says Michael Stow, senior director of global marketing for Hologic. “We anticipate continuing to see a rise in adoption rates as more clinical research is published, especially for physicians with patients who are especially concerned with radiation dose."
In May of last year, Siemens Healthineers received FDA clearance for the use of 3D-only screening mammography utilizing the company’s Mammomat Inspiration with Tomosynthesis Option digital mammography system.
The approval followed a study in which radiologists read 3-D-only images as well as 2-D and 3-D images. The participating doctors decreased average recall rates by an average of 19 percent without the need for a 2-D image.
“Siemens Healthineers is actively promoting this method of screening,” says Jennifer Okken, women’s health specialist at Siemens Healthineers North America. “We do see a future with 3-D-only screening.”
Because tomosynthesis is still an evolving technology, radiologists are still dependent on the support of the 2-D acquisition, particularly for comparison, Okken says.
“I do see that as time moves on and radiologists become more familiar with 3-D-only breast imaging, there won’t be a need for the 2-D projection,” Okken says.
Advancing tomo adoption as 2-D slows
Proponents of digital breast tomosynthesis point to how it leads to decreased recall rates and false positives – benefits that yield more efficient care delivery and a better patient experience. Dr. David Gruen, director of women's imaging and co-director of the Breast Center at Stamford Health in Stamford, Conn., calls digital breast tomosynthesis the “modern-day holy grail of screening.”
Before screening with tomosynthesis, most radiologists were recalling 10 to 20 percent of their screening patients. In Gruen's practice, adopting tomosynthesis almost instantaneously decreased recalls by 45 percent, he says, while the cancer detection rate increased from 4 to 5.6 per 1,000 women, and the cancers that were detected, on average, were smaller.
“I think the slower adoption is almost completely driven by payers,” Gruen says. “People don’t want to invest in technology when they’re not going to get paid.”
In addition to reimbursement concerns, tomosynthesis exposes patients to a higher dose of radiation than 2-D mammography on its own. For radiologists, it also takes longer to read since there are 60 to 80 images for each exam.
Since there are fewer false positives, Gruen says the decrease in unnecessary callbacks opens up time to look at the tomosynthesis images and dedicate more time to care for the women who have real abnormalities.
Agnes Berzsenyi, president and chief executive officer of women’s health for GE Healthcare, says 26 percent of radiologists have adopted digital breast tomosynthesis. While Medicare and a few private insurance companies cover the exam, and three states — Illinois, New York and Pennsylvania — require coverage for tomosynthesis, data show that only 35 to 40 percent of women eligible for screening have coverage for tomosynthesis.
“Minimizing the economic barriers is going to be key in driving adoption,” Berzsenyi says.
The U.S. market for 2-D mammography is down about 10 percent due to the adoption of digital breast tomosynthesis, which is up about 13 percent, according to Berzsenyi. “This gap will continue to grow given the benefits of DBT, changing reimbursement, education and continued technology innovation,” she predicts.
Help from CAD
Computer-aided diagnosis (CAD) for tomosynthesis is also poised to assist radiologists in assessing 3-D images. iCAD recently released one of the industry’s first tomosynthesis (CAD) solutions in the U.S. market. While it can only be used with GE’s SenoClaire 3D Breast Tomosynthesis system and the new Senographe Pristina, iCAD is working on developing technology that can be used with scanners from other manufacturers, says Rodney Hawkins, vice president of marketing for iCAD.
The CAD solution for tomosynthesis is different from traditional CAD in that it has been approved for use concurrently during the primary read of the images, says Hawkins, as opposed to a second-read solution for 2-D images, with marks on the image.
“The radiologist won’t see CAD marks on the images,” he adds. “What they’re seeing are the actual suspicious findings as they appear in the tomosynthesis data. They’re not overly influenced by false positive marks.”
Hawkins says the technology also serves as a workflow efficiency tool to improve reading time — a common complaint among radiologists when reading tomosynthesis.
“Radiologists aren’t getting paid much more to read tomosynthesis images,” Hawkins says. “Our goal with the initial version was to create a workflow tool to help the radiologists rapidly get to what they need to spend their time looking at. Our algorithm runs on the tomo planes data and finds regions of interest.”
The CAD findings are blended into the 2-D synthetic image, which the radiologist uses to navigate into the tomo planes where the findings were detected.
“It saves them having to navigate through looking through every image two or three times sometimes, and creates a nice navigation tool,” Hawkins says.
The company built the tomosynthesis algorithm on “deep learning” technology,using actual patient data to train the algorithm on what the characteristics of a cancer are, “much like a radiologist,” Hawkins says. The technology is detecting more than 92 percent of soft tissue density cancers, versus around 85 percent detected for 2-D mammography CAD.
In Europe, the company has several sites live and one up and running in the U.S., with five sites that have ordered the product.
With the rise of digital breast tomosynthesis, iCAD has not seen a significant amount of growth for its 2-D mammography products.
“Clearly there’s a trend in the U.S. to move to tomosynthesis for primary screening,” Hawkins says. “About a third of the U.S. market has already adopted tomo, according to the latest Mammography Quality Standards Act data.”
What’s new
Further highlighting that tomo is where the growth is, recent new releases from manufacturers center on the 3-D technology.
In April, Siemens Healthineers received FDA clearance for its High Definition Breast Tomosynthesis feature on its Mammomat Inspiration scanner.
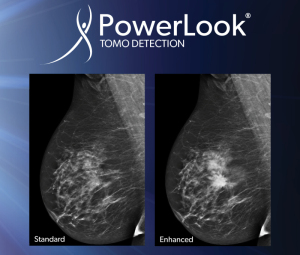
This form of tomosynthesis uses technology called Enhanced Multiple Parameter Iterative Reconstruction, or EMPIRE, a combination of iterative and machine learning algorithms that enhances the contrast of the tomosynthesis image.
Siemens also now provides a synthetic 2-D image, Insight 2D, which Okken says is acquired and reconstructed at the same microns and technical specifications as the tomosynthesis image.
In March, GE Healthcare received FDA clearance for its Senographe Pristina digital breast tomosynthesis scanner. Berzsenyi says the new scanner has a thinner bucky with less hard material, designed to provide a more comfortable experience for patients.
GE also improved the workflow, removing unnecessary repetitive tasks and adding more automation.
The Christine E. Lynn Women’s Health and Wellness Institute in Boca Raton, Fla., recently installed the Senographe Pristina and GE’s SensorySuite, which displays images and sounds of calming scenes, such as beaches or waterfalls, and dispenses calming scents, to create a more relaxing experience for the patient.
Dr. Kathy Schilling, the center’s medical director, and Nicole Coates, a radiologic technologist, say the combination of the new scanner and suite has made the exams much more comfortable for patients.
With curved corners, the scanner doesn’t dig into the patient’s armpit and upper abdomen. Patients don’t hold onto a handle during the exam, and because their muscles are not contracted, there is less pain during compression. The exposure is also shorter with the Pristina.
“The patients are telling us it’s the most comfortable mammogram they’ve ever had,” Coates says.
More relaxed patients lead to better images.
“We’ve found that we’re able to get more breast tissue on the mammogram because the patients are more relaxed,” Schilling says. “We’re using this for all our baseline patients. We don’t want them to have to experience a standard mammogram.”
The system is also easier for technologists to use, Coates says. She is able to switch between the 2-D and 3-D image with one click and she finds that it’s easier to get higher-quality images of breasts with implants earlier in the exam.
The X-ray tube also moves out of the way for the MLO view, so the technologist doesn’t have to bend over, Coates says.
“As a tech, you either learn to position yourself to the side of the patient, or most of us crouch down,” Coates says. “So this is ergonomically better for the tech.”
While Philips Healthcare does not have a tomosynthesis scanner on the market, the company is looking to get a CE mark for its MicroDose 3D, a tomosynthesis scanner that uses a photon-counting technology first developed in Sweden by Sectra, before its mammography business was acquired by Philips in 2011.
The photon-counting technology is expected to enable the MicroDose 3D to provide imaging with lower-dose exposure than conventional tomosynthesis, says Jonas Rehn, the senior product manager for mammography at Philips Healthcare.
The company shared some of the preliminary results from ongoing clinical trials at ECR in Vienna this past March, indicating the decreased dose. “We believe that with this technology we will overcome some of the roadblocks [for tomosynthesis],” Rehn says.
Tomo in the operating room
Tomosynthesis is also moving into the OR.
Kubtec recently released an intraoperative tomosynthesis scanner designed to be used during lumpectomies. Called the MOZART System, it provides a better view of specimen anatomy and microcalcifications than 2-D specimen mammography and reduces surgical recalls, says John Leach, director of marketing for Kubtec.
“When you do mammography for screening, you’re looking to identify if a tumor is there and where it is,” Leach says. “During a procedure, the surgeon knows that the tumor is there. They need to be sure they have removed it entirely. 3-D tomosynthesis simply gives a better view of these crucial surgical margins [than] the traditional 2-D view."
A study of more than 200 patients out of the University of Washington showed that the MOZART System, which was FDA approved in 2015, reduced re-incision rates from 16 percent to 9 percent from 2015 to 2016.
“Re-incisions in the U.S. run at about 30 percent,” Leach says. “Three patients in 10 have to come back and have a second surgery. The battle is on to reduce that number because hospitals are being rated now on performance indicators such as avoiding re-hospitalizations and patient satisfaction.”
For specimen mammography, the tumor and surrounding normal tissue are X-rayed after removal to ensure no cancer cells remain at the outer edge of tissue.
“There are more margins that you can see with the 3-D tomo than with the 2-D mammogram,” says Dr. Cary Kaufman, associate clinical professor of surgery at the Bellingham Breast Center in Bellingham, Wash., who recently began using the MOZART System. “A 2-D image just gives you two silhouettes 90 degrees apart. It doesn’t give you the depth or the third dimension. I can be a better surgeon when I have more information than when I have less information.”
Most facilities that screen with tomosynthesis also capture an image via 2-D mammography, in order to give radiologists a look at the entire breast, as well as the individual layers of the breast that tomosynthesis provides.
A few facilities have been studying a new technique that uses the data obtained during tomosynthesis imaging and compresses it to create a synthesized 2-D-like composite image. This, in turn, lowers the radiation dose, as a woman does not need a mammogram in addition to tomosynthesis, which exposes patients to more radiation than digital mammography.
In a study published last year in the journal Radiology, radiologists at the University of Pennsylvania compared recall rates, biopsy rates, cancer detection rates and radiation dose for more than 15,000 women screened with digital mammography and digital breast tomosynthesis between October 2011 and February 2013, as well as more than 5,000 women screened with digital breast tomosynthesis and synthesized 2-D mammography from January to June 2015.
The study found no significant difference in cancer detection rate for synthesized 2-D mammography and digital breast tomosynthesis versus digital mammography and tomosynthesis, while the average radiation dose was nearly 40 percent lower when the synthetic image was used.
The biopsy rate was also lower when synthesized 2-D mammography was used — 1.3 percent versus 2 percent for the digital mammography and tomosynthesis combination.
“We’ve shown it’s adequate,” says Emily Conant, chief of the division of breast imaging at the Hospital of the University of Pennsylvania and an author of the study. “It further reduces false positives and kept the cancer detection rate the same. If we can create a lower-dose, better mammogram, that’s better.”
Conant says that the 2-D picture is important for looking at a woman’s overall breast density and that some suspicious findings, such as calcium deposits, are more easily seen on a 2-D image. And while some radiologists don’t think the appearance of the synthetic image is as good as a standard 2-D mammogram image, Conant believes the synthesized 2-D mammography and tomosynthesis combination is the future of breast cancer screening.
“In the six years since we’ve implemented tomosynthesis in our clinics, we’ve really seen the impact that it makes,” Conant says. “This whole concept of synthetic imaging is the new kid on the block and it continues to improve. It’s evolving so rapidly. It can only get better.”
Digital breast tomosynthesis scanners from Hologic, GE Healthcare and Siemens Healthineers are all capable of providing the synthesized 2-D image.
Other clinicians have similarly shown that the synthesized 2-D image is adequate.
For a study published in the journal Radiology in February, researchers at the Christiana Care Health System’s Helen F. Graham Cancer Center & Research Institute looked at more than 32,000 women screened with just mammography, more than 30,000 screened with a combination of tomosynthesis and mammography and more than 16,000 women screened using the synthesized 2-D mammography over five years, a much larger sample size than previous studies.
The recall rate for synthesized 2-D mammography was 4.3 percent, compared to 5.8 percent for tomosynthesis and mammography and 8.7 percent for the 2-D mammography alone. More than 76 percent of invasive cancers were detected using synthesized 2-D mammography, versus more than 61 percent for tomosynthesis and mammography.
Using the synthesized 2-D mammography also decreased the radiation dose between 40 and 45 percent, says Dr. Jacqueline S. Holt, director of breast imaging at the Christiana Care Health System’s Helen F. Graham Cancer Center & Research Institute.
“I was hoping that this article showing performance in a real-world setting would tilt the dials,” Holt says. “The dose is down to where digital [mammography] was, plus we have the benefit of the 3-D images, plus we have the 2-D image. I think that this will be the new normal mammogram.”
Debra Monticciolo, chair of the American College of Radiology’s Commission on Breast Imaging, says that while preliminary results have shown that the synthesized 2-D image is equally diagnostic, she looks forward to the results of more studies on its use.
“We still do the standard digital mammography and add tomosynthesis to it,” says Monticciolo, who is also vice chair for research and section chief of breast imaging in the department of radiology at Baylor Scott & White Healthcare in Temple, Texas. “That’s the way we started and there wasn’t enough data yet to go with the composite. The composite has a different look than the standard 2-D image, which breast imagers will likely get used to over time.”
But even Monticciolo believes it will be a more common practice to use the synthesized image in the future.
“Over time, companies work on algorithms,” Monticciolo says. “Over time it will also improve.”
Hologic's C-View software, allowing radiologists to generate a 2-D image from the tomosynthesis dataset, has been available since February 2011.
“We've seen an increase in adoption rates as more and more clinical research is released demonstrating comparable invasive cancer detection rates and recall rates to traditional breast tomosynthesis screening exams,” says Michael Stow, senior director of global marketing for Hologic. “We anticipate continuing to see a rise in adoption rates as more clinical research is published, especially for physicians with patients who are especially concerned with radiation dose."
In May of last year, Siemens Healthineers received FDA clearance for the use of 3D-only screening mammography utilizing the company’s Mammomat Inspiration with Tomosynthesis Option digital mammography system.
The approval followed a study in which radiologists read 3-D-only images as well as 2-D and 3-D images. The participating doctors decreased average recall rates by an average of 19 percent without the need for a 2-D image.
“Siemens Healthineers is actively promoting this method of screening,” says Jennifer Okken, women’s health specialist at Siemens Healthineers North America. “We do see a future with 3-D-only screening.”
Because tomosynthesis is still an evolving technology, radiologists are still dependent on the support of the 2-D acquisition, particularly for comparison, Okken says.
“I do see that as time moves on and radiologists become more familiar with 3-D-only breast imaging, there won’t be a need for the 2-D projection,” Okken says.
Advancing tomo adoption as 2-D slows
Proponents of digital breast tomosynthesis point to how it leads to decreased recall rates and false positives – benefits that yield more efficient care delivery and a better patient experience. Dr. David Gruen, director of women's imaging and co-director of the Breast Center at Stamford Health in Stamford, Conn., calls digital breast tomosynthesis the “modern-day holy grail of screening.”
Before screening with tomosynthesis, most radiologists were recalling 10 to 20 percent of their screening patients. In Gruen's practice, adopting tomosynthesis almost instantaneously decreased recalls by 45 percent, he says, while the cancer detection rate increased from 4 to 5.6 per 1,000 women, and the cancers that were detected, on average, were smaller.
“I think the slower adoption is almost completely driven by payers,” Gruen says. “People don’t want to invest in technology when they’re not going to get paid.”
In addition to reimbursement concerns, tomosynthesis exposes patients to a higher dose of radiation than 2-D mammography on its own. For radiologists, it also takes longer to read since there are 60 to 80 images for each exam.
Since there are fewer false positives, Gruen says the decrease in unnecessary callbacks opens up time to look at the tomosynthesis images and dedicate more time to care for the women who have real abnormalities.
Agnes Berzsenyi, president and chief executive officer of women’s health for GE Healthcare, says 26 percent of radiologists have adopted digital breast tomosynthesis. While Medicare and a few private insurance companies cover the exam, and three states — Illinois, New York and Pennsylvania — require coverage for tomosynthesis, data show that only 35 to 40 percent of women eligible for screening have coverage for tomosynthesis.
“Minimizing the economic barriers is going to be key in driving adoption,” Berzsenyi says.
The U.S. market for 2-D mammography is down about 10 percent due to the adoption of digital breast tomosynthesis, which is up about 13 percent, according to Berzsenyi. “This gap will continue to grow given the benefits of DBT, changing reimbursement, education and continued technology innovation,” she predicts.
Help from CAD
Computer-aided diagnosis (CAD) for tomosynthesis is also poised to assist radiologists in assessing 3-D images. iCAD recently released one of the industry’s first tomosynthesis (CAD) solutions in the U.S. market. While it can only be used with GE’s SenoClaire 3D Breast Tomosynthesis system and the new Senographe Pristina, iCAD is working on developing technology that can be used with scanners from other manufacturers, says Rodney Hawkins, vice president of marketing for iCAD.
The CAD solution for tomosynthesis is different from traditional CAD in that it has been approved for use concurrently during the primary read of the images, says Hawkins, as opposed to a second-read solution for 2-D images, with marks on the image.
“The radiologist won’t see CAD marks on the images,” he adds. “What they’re seeing are the actual suspicious findings as they appear in the tomosynthesis data. They’re not overly influenced by false positive marks.”
Hawkins says the technology also serves as a workflow efficiency tool to improve reading time — a common complaint among radiologists when reading tomosynthesis.
“Radiologists aren’t getting paid much more to read tomosynthesis images,” Hawkins says. “Our goal with the initial version was to create a workflow tool to help the radiologists rapidly get to what they need to spend their time looking at. Our algorithm runs on the tomo planes data and finds regions of interest.”
The CAD findings are blended into the 2-D synthetic image, which the radiologist uses to navigate into the tomo planes where the findings were detected.
“It saves them having to navigate through looking through every image two or three times sometimes, and creates a nice navigation tool,” Hawkins says.
The company built the tomosynthesis algorithm on “deep learning” technology,using actual patient data to train the algorithm on what the characteristics of a cancer are, “much like a radiologist,” Hawkins says. The technology is detecting more than 92 percent of soft tissue density cancers, versus around 85 percent detected for 2-D mammography CAD.
In Europe, the company has several sites live and one up and running in the U.S., with five sites that have ordered the product.
With the rise of digital breast tomosynthesis, iCAD has not seen a significant amount of growth for its 2-D mammography products.
“Clearly there’s a trend in the U.S. to move to tomosynthesis for primary screening,” Hawkins says. “About a third of the U.S. market has already adopted tomo, according to the latest Mammography Quality Standards Act data.”
What’s new
Further highlighting that tomo is where the growth is, recent new releases from manufacturers center on the 3-D technology.
In April, Siemens Healthineers received FDA clearance for its High Definition Breast Tomosynthesis feature on its Mammomat Inspiration scanner.
This form of tomosynthesis uses technology called Enhanced Multiple Parameter Iterative Reconstruction, or EMPIRE, a combination of iterative and machine learning algorithms that enhances the contrast of the tomosynthesis image.
Siemens also now provides a synthetic 2-D image, Insight 2D, which Okken says is acquired and reconstructed at the same microns and technical specifications as the tomosynthesis image.
In March, GE Healthcare received FDA clearance for its Senographe Pristina digital breast tomosynthesis scanner. Berzsenyi says the new scanner has a thinner bucky with less hard material, designed to provide a more comfortable experience for patients.
GE also improved the workflow, removing unnecessary repetitive tasks and adding more automation.
The Christine E. Lynn Women’s Health and Wellness Institute in Boca Raton, Fla., recently installed the Senographe Pristina and GE’s SensorySuite, which displays images and sounds of calming scenes, such as beaches or waterfalls, and dispenses calming scents, to create a more relaxing experience for the patient.
Dr. Kathy Schilling, the center’s medical director, and Nicole Coates, a radiologic technologist, say the combination of the new scanner and suite has made the exams much more comfortable for patients.
With curved corners, the scanner doesn’t dig into the patient’s armpit and upper abdomen. Patients don’t hold onto a handle during the exam, and because their muscles are not contracted, there is less pain during compression. The exposure is also shorter with the Pristina.
“The patients are telling us it’s the most comfortable mammogram they’ve ever had,” Coates says.
More relaxed patients lead to better images.
“We’ve found that we’re able to get more breast tissue on the mammogram because the patients are more relaxed,” Schilling says. “We’re using this for all our baseline patients. We don’t want them to have to experience a standard mammogram.”
The system is also easier for technologists to use, Coates says. She is able to switch between the 2-D and 3-D image with one click and she finds that it’s easier to get higher-quality images of breasts with implants earlier in the exam.
The X-ray tube also moves out of the way for the MLO view, so the technologist doesn’t have to bend over, Coates says.
“As a tech, you either learn to position yourself to the side of the patient, or most of us crouch down,” Coates says. “So this is ergonomically better for the tech.”
While Philips Healthcare does not have a tomosynthesis scanner on the market, the company is looking to get a CE mark for its MicroDose 3D, a tomosynthesis scanner that uses a photon-counting technology first developed in Sweden by Sectra, before its mammography business was acquired by Philips in 2011.
The photon-counting technology is expected to enable the MicroDose 3D to provide imaging with lower-dose exposure than conventional tomosynthesis, says Jonas Rehn, the senior product manager for mammography at Philips Healthcare.
The company shared some of the preliminary results from ongoing clinical trials at ECR in Vienna this past March, indicating the decreased dose. “We believe that with this technology we will overcome some of the roadblocks [for tomosynthesis],” Rehn says.
Tomo in the operating room
Tomosynthesis is also moving into the OR.
Kubtec recently released an intraoperative tomosynthesis scanner designed to be used during lumpectomies. Called the MOZART System, it provides a better view of specimen anatomy and microcalcifications than 2-D specimen mammography and reduces surgical recalls, says John Leach, director of marketing for Kubtec.
“When you do mammography for screening, you’re looking to identify if a tumor is there and where it is,” Leach says. “During a procedure, the surgeon knows that the tumor is there. They need to be sure they have removed it entirely. 3-D tomosynthesis simply gives a better view of these crucial surgical margins [than] the traditional 2-D view."
A study of more than 200 patients out of the University of Washington showed that the MOZART System, which was FDA approved in 2015, reduced re-incision rates from 16 percent to 9 percent from 2015 to 2016.
“Re-incisions in the U.S. run at about 30 percent,” Leach says. “Three patients in 10 have to come back and have a second surgery. The battle is on to reduce that number because hospitals are being rated now on performance indicators such as avoiding re-hospitalizations and patient satisfaction.”
For specimen mammography, the tumor and surrounding normal tissue are X-rayed after removal to ensure no cancer cells remain at the outer edge of tissue.
“There are more margins that you can see with the 3-D tomo than with the 2-D mammogram,” says Dr. Cary Kaufman, associate clinical professor of surgery at the Bellingham Breast Center in Bellingham, Wash., who recently began using the MOZART System. “A 2-D image just gives you two silhouettes 90 degrees apart. It doesn’t give you the depth or the third dimension. I can be a better surgeon when I have more information than when I have less information.”