3-D bioprinting’s lifesaving potential
January 24, 2018
By Steven Morris
The heart is one of the most important organs in the human body, and nobody can survive without one. However, it is possible to survive without your own heart, long as you receive a functional one to replace it.
On December 3, 1967, Dr. Christiaan Barnard performed the first successful human-to-human heart transplant on 53-year old Lewis Washkansky, a South African grocer dying of heart disease. Although Washkansky died 18 days later from pneumonia, his new heart functioned normally until his death, foreshadowing innovation within this lifesaving procedure.
Much progress has been made in heart transplants since then, but even so, only half of the heart transplant recipients lucky enough to receive a donor heart live longer than 10 years. Perhaps the biggest problem now is not in the operating room, but in the very finite supply of, and seemingly endless demand for, hearts. At any given time, there are over 100,000 Americans alone on the waiting list to receive heart transplants, but only about 2,000 heart transplants are performed in the U.S. each year. That means an alarmingly low 2% of the demand is met. In this era of medicine, a 98% failure rate is simply unacceptable.
Organ rejection is also an obstacle that the transplant industry must overcome. This is when an organ recipient’s immune system recognizes a transplanted organ as foreign and attacks it, intending to protect the body. This occurs when the cells of the transplanted organs are not close enough of a match to the recipient’s. With that said, transplanting patient-specific organs – or as close to them as possible – is crucial.
Despite all of world medicine’s progress, there has not yet been a solution to this supply-and-demand problem. While individuals take whatever measures they can to improve their heart health and avoid becoming part of the demand, the medical field is looking to 3-D bioprinting as a means of increasing the supply of available organs.
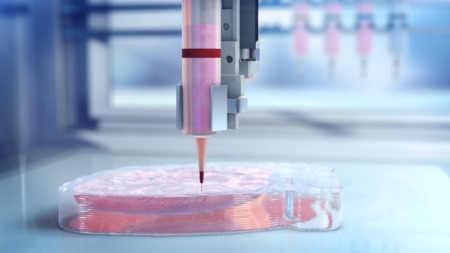
3-D bioprinting is the process of creating cell patterns in a confined space using 3-D printing technologies, thereby preserving cell function and viability within the printed construct. More simply, a 3-D bioprinter is a specialized 3-D printer developed to protect living cells during printing. Now bioprinters can create functional biological structures to potentially restore, maintain, improve, or even replace existing organ function.
3-D bioprinting may seem like a “next generation” concept, but so, too, did many medical advancements and achievements throughout the course of human history. In fact, for some time now, scientists and engineers have used 3-D printers to create objects from metals and plastics, in an industry projected to be worth nearly $33 billion by 2023. Printing inanimate objects has its use, but what if we could print functional human organs? It may sound like science fiction, but it’s science fact.
The 3-D bioprinting process – of a heart, for example – begins with MR creating a detailed three-dimensional image of a patient’s heart. Computer software uses this image to construct a digital model of a new heart for the patient, featuring the original shape and size. After safely extracting cells from the patient through a blood sample, those blood cells are reprogrammed and converted into specialized heart cells, leveraging recent stem cell developments. Then, a “bio-ink” is created using the specialized heart cells, nutrients, and other materials that will help the cells survive the bioprinting process.
As you can imagine, the bioprinting is done with a 3-D bioprinter, using the dimensions from the MR. After printing, the heart is matured in a bioreactor, made stronger and readied for transplant. This process also eliminates the chance of organ rejection, since the transplantable organ is made of the recipient’s own cells, meaning it will be recognized as the patient’s own organ and not as foreign.
While only about 2,000 heart transplants occur in the U.S. each year, 2017 saw nearly 35,000 transplants of various organs, and only a little more than 16,000 donors. It seems that not only with hearts, but with organs as a whole, the transplant-ready supply is well short of the demand. The good news is that the 3-D bioprinting process has the potential to create a wealth of organs in addition to hearts, and thus the potential to save even more lives. The more the technology matures, the more types of organs it will be able to print, and the more lives it will be able to save.
The ability to create transplantable organs represents tremendous opportunities in medicine, from both financial and humanitarian standpoints. We’ve outlined the market opportunity of the 3-D printing industry as a whole, and 3-D bioprinting is surely a significant portion of that projection. Market opportunities are always great, but what’s really exciting is that the number of lives we can save is only limited by the organs we can produce. With hundreds of thousands of people dying annually because of the shortfall of available organs, this is not just an opportunity, but a responsibility.
About the Author: Steven Morris is the CEO of BIOLIFE4D, a pioneering biotech company laser-focused on leveraging advances in life sciences and tissue engineering to 3-D bioprint a viable human heart suitable for transplant.
The heart is one of the most important organs in the human body, and nobody can survive without one. However, it is possible to survive without your own heart, long as you receive a functional one to replace it.
On December 3, 1967, Dr. Christiaan Barnard performed the first successful human-to-human heart transplant on 53-year old Lewis Washkansky, a South African grocer dying of heart disease. Although Washkansky died 18 days later from pneumonia, his new heart functioned normally until his death, foreshadowing innovation within this lifesaving procedure.
Much progress has been made in heart transplants since then, but even so, only half of the heart transplant recipients lucky enough to receive a donor heart live longer than 10 years. Perhaps the biggest problem now is not in the operating room, but in the very finite supply of, and seemingly endless demand for, hearts. At any given time, there are over 100,000 Americans alone on the waiting list to receive heart transplants, but only about 2,000 heart transplants are performed in the U.S. each year. That means an alarmingly low 2% of the demand is met. In this era of medicine, a 98% failure rate is simply unacceptable.
Organ rejection is also an obstacle that the transplant industry must overcome. This is when an organ recipient’s immune system recognizes a transplanted organ as foreign and attacks it, intending to protect the body. This occurs when the cells of the transplanted organs are not close enough of a match to the recipient’s. With that said, transplanting patient-specific organs – or as close to them as possible – is crucial.
Despite all of world medicine’s progress, there has not yet been a solution to this supply-and-demand problem. While individuals take whatever measures they can to improve their heart health and avoid becoming part of the demand, the medical field is looking to 3-D bioprinting as a means of increasing the supply of available organs.
3-D bioprinting is the process of creating cell patterns in a confined space using 3-D printing technologies, thereby preserving cell function and viability within the printed construct. More simply, a 3-D bioprinter is a specialized 3-D printer developed to protect living cells during printing. Now bioprinters can create functional biological structures to potentially restore, maintain, improve, or even replace existing organ function.
3-D bioprinting may seem like a “next generation” concept, but so, too, did many medical advancements and achievements throughout the course of human history. In fact, for some time now, scientists and engineers have used 3-D printers to create objects from metals and plastics, in an industry projected to be worth nearly $33 billion by 2023. Printing inanimate objects has its use, but what if we could print functional human organs? It may sound like science fiction, but it’s science fact.
The 3-D bioprinting process – of a heart, for example – begins with MR creating a detailed three-dimensional image of a patient’s heart. Computer software uses this image to construct a digital model of a new heart for the patient, featuring the original shape and size. After safely extracting cells from the patient through a blood sample, those blood cells are reprogrammed and converted into specialized heart cells, leveraging recent stem cell developments. Then, a “bio-ink” is created using the specialized heart cells, nutrients, and other materials that will help the cells survive the bioprinting process.
As you can imagine, the bioprinting is done with a 3-D bioprinter, using the dimensions from the MR. After printing, the heart is matured in a bioreactor, made stronger and readied for transplant. This process also eliminates the chance of organ rejection, since the transplantable organ is made of the recipient’s own cells, meaning it will be recognized as the patient’s own organ and not as foreign.
While only about 2,000 heart transplants occur in the U.S. each year, 2017 saw nearly 35,000 transplants of various organs, and only a little more than 16,000 donors. It seems that not only with hearts, but with organs as a whole, the transplant-ready supply is well short of the demand. The good news is that the 3-D bioprinting process has the potential to create a wealth of organs in addition to hearts, and thus the potential to save even more lives. The more the technology matures, the more types of organs it will be able to print, and the more lives it will be able to save.
The ability to create transplantable organs represents tremendous opportunities in medicine, from both financial and humanitarian standpoints. We’ve outlined the market opportunity of the 3-D printing industry as a whole, and 3-D bioprinting is surely a significant portion of that projection. Market opportunities are always great, but what’s really exciting is that the number of lives we can save is only limited by the organs we can produce. With hundreds of thousands of people dying annually because of the shortfall of available organs, this is not just an opportunity, but a responsibility.
About the Author: Steven Morris is the CEO of BIOLIFE4D, a pioneering biotech company laser-focused on leveraging advances in life sciences and tissue engineering to 3-D bioprint a viable human heart suitable for transplant.