Construction costs for proton therapy facilities can exceed $100 million, but single gantry systems have emerged as a less expensive alternative.
Improving pediatric access to proton therapy
April 06, 2020
by John R. Fischer, Senior Reporter
A six-year-old boy underwent multiple surgeries to treat a malignant brain tumor but the disease kept coming back. It wasn’t until the child underwent proton therapy at the Medical Institute of Berezin Sergey in St. Petersburg, Russia, that the cancer was fully eradicated and he could get back to having a regular life.
“Before, he would have three surgeries every three or four months,” Dr. Arkadi Stolpner, owner of the institute, told HCB News. “The tumor continued to grow. We treated this boy, and now two years later he is tumor free. There are no more surgeries needed because nothing is growing.”
Stories like that are not uncommon. As proton therapy adoption increases, the body of evidence shows that for many cancers, there is no better treatment available. That’s why major cities around the world, such as New York, Madrid, and Chennai have all opened up proton therapy facilities in the last two years.
For pediatric patients specifically, the advantages of better outcomes and fewer side effects mean improved quality of life for many decades to come. Ensuring these young patients have access to proton therapy, however, is a challenge in its own right with a range of unique obstacles.
Logistical challenges at home and abroad
Despite increased investment in proton therapy in recent years, there are still fewer than 90 facilities in the world, according to the Particle Therapy Co-Operative Group (PTCOG). For the vast majority of pediatric patients, receiving treatment requires traveling long distances, making lodging arrangements and potential time off work for the parents who come along.
“It’s really important that centers have housing options for patients,” said Dr. Stephanie Perkins, associate professor in the department of radiation oncology at Washington University School of Medicine. “We are very fortunate to have the Ronald McDonald House, which offers free lodging for patients. There is still the cost of car transportation but we’re also very fortunate to have some resources to provide funds to patients for travel. Reimbursements for travel and lodging are typically not included in U.S. healthcare coverage plans.”
At the Medical Institute of Berezin Sergey, where the majority of patients treated are children, Stolpner said a 60-bed hospital is being finalized this year to house patients and also provide beds to at least one parent of the patient.
In the Netherlands, proton therapy is covered by the government and the costs of travel and accommodation are fully reimbursed, according to Dr. Hans Langendijk, professor and chair of the department of radiation oncology at University Medical Center Groningen. Centers are also required to offer lodging to patients.
“There are countries where proton therapy facilities are not available and only a limited number of patients are referred for proton therapy,” he said. “This is a typical example where cross border healthcare could play a very important role and also to make proton therapy available for pediatric patients that come from other countries. It remains difficult in clinical practice to obtain those referrals for legal, practice and logistical reasons, and discussions with insurance companies.”
While access to proton therapy is limited throughout the world, there are considerably more facilities in the U.S. than anywhere else. At present, there are approximately 30 proton therapy providers across the country, a number which has risen with the emergence of smaller footprint, single-gantry solutions.
Historically, proton therapy centers have been multi-gantry facilities operated by a high-volume academic health system. As the smaller units gain ground, access enters new regions and brings access to new populations.
Reducing the need for anesthesia
A typical proton therapy treatment takes three-to-six weeks and consists of several sessions where the patient must remain still for 15-30 minutes. For young kids, anesthesia is often the only way to ensure they will remain motionless during treatment, but it comes with drawbacks.
“The anesthesia requires that children receive treatment in the morning on an empty stomach, so they end up missing breakfast,” said Washington University’s Perkins. “A procedure that would typically take 20 minutes ends up taking an hour to an hour and a half because kids require sedation and then recovery from sedation. They are sometimes irritable when they wake up from sedation, and they can miss half the day just from recovering from treatment. For the kids who can do it awake, they can actually go to school for the day and receive their treatment in the afternoon.”
Using tactics similar to those deployed the MR imaging suite, many proton therapy providers are turning to audio and visual stimulation to help curb the anxiety pediatrics patients may feel in the treatment environment. Perkins and his colleagues are currently participating in a trial conducted by Stanford University to weigh the advantages of incorporating movies into proton therapy as a way to distract children and keep them entertained.
At the Medical Institute of Berezin Sergey in St. Petersburg, patients can look out the window and watch real live monkeys playing in an enclosed habitat. Looking at the animals transports pediatric patients from a place that may be frightening and intimidating to a private zoo exhibit. “They feel better because the monkeys make them feel it’s not a scary place,” said Stolpner, adding that the distraction ultimately allows for more efficient treatment.
Although less exotic, another tactic for reducing the need for anesthesia is to enlist child life specialists trained to communicate with young patients and their families about what to expect during the proton therapy experience. In some cases, these professionals can help children understand why it is better to be brave and remain still than to request anesthesia.
“Certified child life specialists have an integral role in reducing the number of children who need anesthesia,” said Jennifer Maggiore, executive director of the National Association of Proton Therapy. “You also must have care coordination by nurse navigators and oncology social workers to ensure children receive comprehensive cancer care and adequate resources throughout their treatment.”
Insurance coverage and clear communication
Payors in the U.S. have been increasingly cooperative about covering proton treatment for pediatric patients who will benefit the most from having it.
“Children have much longer to live after cancer treatment so survivorship in many ways is kind of more important if you are looking at 80 years of survival,” said Dr. Christine Hill-Kayser, chief of pediatric radiation oncology at Children’s Hospital of Philadelphia. “In addition, we know that normal tissue in kids is more sensitive to damage from radiation. These two factors together increase national recognition of the need for this technology.”
On the other hand, not every pediatric cancer patient is a good candidate for proton therapy, so it’s important for referring physicians to be able to explain their reasoning. Parents (and patients) are increasingly seeking medical advice online so there will be cases where a family seeks proton therapy even though conventionally radiation therapy offers comparable outcomes with less difficulty.
“There are times in my opinion where it is optimal to have a patient treated on a therapeutic photon machine where the treatment can be delivered more efficiently for them,” said Hill-Kayser. “The treatment may be quicker and easier to tolerate so fewer kids need anesthesia with X-rays.”
Toward better access, better techniques
Pediatric access to proton therapy has improved steadily as evidence recommending the treatment has accrued. Looking toward the future, experts see availability increasing as techniques become more sophisticated and capital expenses come down.
“Advances in technology are reducing the cost of implementing proton therapy in a cancer center or hospital, allowing more patients to have this treatment available closer to their home,” said Maggiore. “As research evolves and demonstrates the value of proton therapy, we will encourage and advise commercial insurers to include proton therapy for more cancer sites in cancer treatment guidelines, ensuring this advanced technology is adopted for more cancer patients.”
As single-gantry facilities continue to open, conventional proton treatments will become more accessible to a greater population, but Dr. Thomas E. Merchant, chair of the department of radiation oncology at St. Jude Children’s Research Hospital, expects that high-volume academic providers will continue to lead the way in managing the more complex cases.
“I think for some diseases, it’s better to be treated at an academic medical center,” said Merchant. “For other conditions or clinical scenarios, it might be fine to be treated closer to home. I think the guidelines for that have yet to be sorted out.”
Expanded access to proton therapy should also have a direct correlation on the number of radiation oncologists who are trained to offer it.
“When physicians are trained in radiation therapy, they’re not trained to use protons unless they’re at a facility with access to it,” said Dr. John Breneman, medical director of the Cincinnati Children' Hospital Medical Center UC Health Proton Therapy Center. “Most major cancer centers now offer proton therapy. But those are still the minority of programs where radiation oncologists are trained.”
Flash therapy, in which large doses of radiation are delivered in a fraction of a second, is also stirring optimism in the proton community. The speed of the dose is expected to help it irradiate tumors while sparing healthy surrounding tissue, and in the process, lower entire treatment time from the typical seven weeks to less than a second. Advocates of the practice say such benefits may ultimately lead to greater access to cancer treatment at lower costs.
“I do hope we will see it in several years clinically,” said Stolpner. “The main thing about Flash is that it will make proton therapy more affordable, because in theory, we will be able to use three or four fractions instead of 30.”
“Before, he would have three surgeries every three or four months,” Dr. Arkadi Stolpner, owner of the institute, told HCB News. “The tumor continued to grow. We treated this boy, and now two years later he is tumor free. There are no more surgeries needed because nothing is growing.”
Stories like that are not uncommon. As proton therapy adoption increases, the body of evidence shows that for many cancers, there is no better treatment available. That’s why major cities around the world, such as New York, Madrid, and Chennai have all opened up proton therapy facilities in the last two years.
For pediatric patients specifically, the advantages of better outcomes and fewer side effects mean improved quality of life for many decades to come. Ensuring these young patients have access to proton therapy, however, is a challenge in its own right with a range of unique obstacles.
Anesthesia is often used to alleviate young children of their anxiety during proton therapy procedures, but lengthens the amount of time required for delivering a course of proton therapy.
Despite increased investment in proton therapy in recent years, there are still fewer than 90 facilities in the world, according to the Particle Therapy Co-Operative Group (PTCOG). For the vast majority of pediatric patients, receiving treatment requires traveling long distances, making lodging arrangements and potential time off work for the parents who come along.
“It’s really important that centers have housing options for patients,” said Dr. Stephanie Perkins, associate professor in the department of radiation oncology at Washington University School of Medicine. “We are very fortunate to have the Ronald McDonald House, which offers free lodging for patients. There is still the cost of car transportation but we’re also very fortunate to have some resources to provide funds to patients for travel. Reimbursements for travel and lodging are typically not included in U.S. healthcare coverage plans.”
At the Medical Institute of Berezin Sergey, where the majority of patients treated are children, Stolpner said a 60-bed hospital is being finalized this year to house patients and also provide beds to at least one parent of the patient.
In the Netherlands, proton therapy is covered by the government and the costs of travel and accommodation are fully reimbursed, according to Dr. Hans Langendijk, professor and chair of the department of radiation oncology at University Medical Center Groningen. Centers are also required to offer lodging to patients.
“There are countries where proton therapy facilities are not available and only a limited number of patients are referred for proton therapy,” he said. “This is a typical example where cross border healthcare could play a very important role and also to make proton therapy available for pediatric patients that come from other countries. It remains difficult in clinical practice to obtain those referrals for legal, practice and logistical reasons, and discussions with insurance companies.”
While access to proton therapy is limited throughout the world, there are considerably more facilities in the U.S. than anywhere else. At present, there are approximately 30 proton therapy providers across the country, a number which has risen with the emergence of smaller footprint, single-gantry solutions.
Historically, proton therapy centers have been multi-gantry facilities operated by a high-volume academic health system. As the smaller units gain ground, access enters new regions and brings access to new populations.
Reducing the need for anesthesia
A typical proton therapy treatment takes three-to-six weeks and consists of several sessions where the patient must remain still for 15-30 minutes. For young kids, anesthesia is often the only way to ensure they will remain motionless during treatment, but it comes with drawbacks.
“The anesthesia requires that children receive treatment in the morning on an empty stomach, so they end up missing breakfast,” said Washington University’s Perkins. “A procedure that would typically take 20 minutes ends up taking an hour to an hour and a half because kids require sedation and then recovery from sedation. They are sometimes irritable when they wake up from sedation, and they can miss half the day just from recovering from treatment. For the kids who can do it awake, they can actually go to school for the day and receive their treatment in the afternoon.”
Using tactics similar to those deployed the MR imaging suite, many proton therapy providers are turning to audio and visual stimulation to help curb the anxiety pediatrics patients may feel in the treatment environment. Perkins and his colleagues are currently participating in a trial conducted by Stanford University to weigh the advantages of incorporating movies into proton therapy as a way to distract children and keep them entertained.
At the Medical Institute of Berezin Sergey in St. Petersburg, patients can look out the window and watch real live monkeys playing in an enclosed habitat. Looking at the animals transports pediatric patients from a place that may be frightening and intimidating to a private zoo exhibit. “They feel better because the monkeys make them feel it’s not a scary place,” said Stolpner, adding that the distraction ultimately allows for more efficient treatment.
The biggest challenge that children face is being within travel distance of a proton therapy center. Many who live far away have to pay what can be steep transport and lodging costs to undergo treatment.
“Certified child life specialists have an integral role in reducing the number of children who need anesthesia,” said Jennifer Maggiore, executive director of the National Association of Proton Therapy. “You also must have care coordination by nurse navigators and oncology social workers to ensure children receive comprehensive cancer care and adequate resources throughout their treatment.”
Insurance coverage and clear communication
Payors in the U.S. have been increasingly cooperative about covering proton treatment for pediatric patients who will benefit the most from having it.
“Children have much longer to live after cancer treatment so survivorship in many ways is kind of more important if you are looking at 80 years of survival,” said Dr. Christine Hill-Kayser, chief of pediatric radiation oncology at Children’s Hospital of Philadelphia. “In addition, we know that normal tissue in kids is more sensitive to damage from radiation. These two factors together increase national recognition of the need for this technology.”
On the other hand, not every pediatric cancer patient is a good candidate for proton therapy, so it’s important for referring physicians to be able to explain their reasoning. Parents (and patients) are increasingly seeking medical advice online so there will be cases where a family seeks proton therapy even though conventionally radiation therapy offers comparable outcomes with less difficulty.
“There are times in my opinion where it is optimal to have a patient treated on a therapeutic photon machine where the treatment can be delivered more efficiently for them,” said Hill-Kayser. “The treatment may be quicker and easier to tolerate so fewer kids need anesthesia with X-rays.”
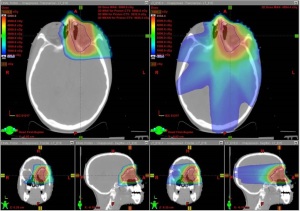
A challenge for small children during proton therapy is keeping absolutely still during proce- dures. Some require anesthesia in order for it to be successful. Courtesy of the department of radiation oncology at Washington University School of Medicine
Pediatric access to proton therapy has improved steadily as evidence recommending the treatment has accrued. Looking toward the future, experts see availability increasing as techniques become more sophisticated and capital expenses come down.
“Advances in technology are reducing the cost of implementing proton therapy in a cancer center or hospital, allowing more patients to have this treatment available closer to their home,” said Maggiore. “As research evolves and demonstrates the value of proton therapy, we will encourage and advise commercial insurers to include proton therapy for more cancer sites in cancer treatment guidelines, ensuring this advanced technology is adopted for more cancer patients.”
As single-gantry facilities continue to open, conventional proton treatments will become more accessible to a greater population, but Dr. Thomas E. Merchant, chair of the department of radiation oncology at St. Jude Children’s Research Hospital, expects that high-volume academic providers will continue to lead the way in managing the more complex cases.
“I think for some diseases, it’s better to be treated at an academic medical center,” said Merchant. “For other conditions or clinical scenarios, it might be fine to be treated closer to home. I think the guidelines for that have yet to be sorted out.”
Expanded access to proton therapy should also have a direct correlation on the number of radiation oncologists who are trained to offer it.
Insurance coverage for pediatric proton therapy has become increasingly available, as evidence has illustrated the quality of life benefits for patients with certain cancers in com- parison to conventional radiation therapy.
Flash therapy, in which large doses of radiation are delivered in a fraction of a second, is also stirring optimism in the proton community. The speed of the dose is expected to help it irradiate tumors while sparing healthy surrounding tissue, and in the process, lower entire treatment time from the typical seven weeks to less than a second. Advocates of the practice say such benefits may ultimately lead to greater access to cancer treatment at lower costs.
“I do hope we will see it in several years clinically,” said Stolpner. “The main thing about Flash is that it will make proton therapy more affordable, because in theory, we will be able to use three or four fractions instead of 30.”