by
Brendon Nafziger, DOTmed News Associate Editor | April 30, 2012
A bill recently introduced into the Senate would block the Centers for Medicare and Medicaid Services from continuing with certain cuts that affect radiologists.
The bill, S. 2347, the Diagnostic Imaging Services Access Protection Act, would prevent CMS from continuing with a 25 percent cut to the professional component to doctors from the same practice who perform multiple MRI, CT or ultrasound scans on the same patient during the same visit.
In order to continue with the reimbursement reductions, the bill requires CMS to order the Institute of Medicine to run a study proving the cuts are worthwhile.



Ad Statistics
Times Displayed: 2003
Times Visited: 8 Fast-moving cardiac structures have a big impact on imaging. Fujifilm’s SCENARIA View premium performance CT brings solutions to address motion in Coronary CTA while delivering unique dose saving and workflow increasing benefits.
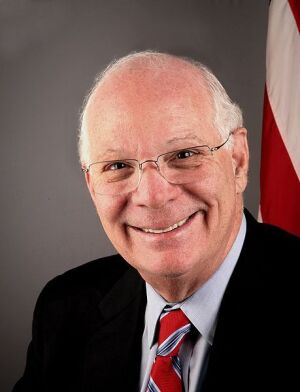
The bill was introduced by Sens. Dave Vitter, a Republican from Louisiana, and Ben Cardin, a Democrat from Maryland. It's a Senate version of House bill HR 3269, introduced by Reps. Peter Olson, a Texas Republican, and Betty McCollum, a Minnesota Democrat, in October. That bill has already gone on to rack up 234 co-sponsors, the American College of Radiology said on its website.
CMS instituted the cuts this year because it said doctors enjoy "efficiencies" when performing multiple scans on the same patient during the same day. Previously, the CMS also cut the technical component for such situations.
But the ACR, which backs the current bill, has maintained that other studies show doctors gain only 5 percent efficiencies when the multiple exams given to the same patient are interpreted, so the cuts are excessive.