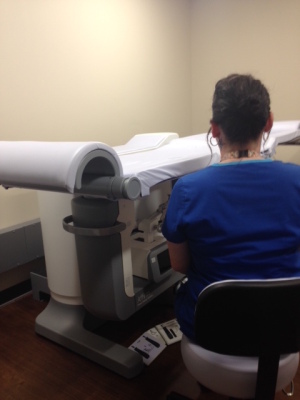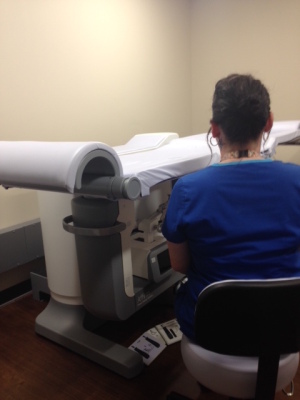
A technologist with the
Affirm prone breast biopsy system
From the July 2017 issue of HealthCare Business News magazine
By Terri-Ann Gizienski
Breast tomosynthesis made headlines in 2011 when the technology first became available, commended for allowing radiologists to more clearly visualize invasive cancers that breast tissue had previously obscured with traditional 2-D imaging, and to differentiate them from benign cysts and lymph nodes that in the past would require additional imaging.
BT is quickly becoming the standard of care and is on its way to becoming the new “gold standard” for breast cancer screening as more women learn about its benefits and more facilities acquire the technology.



Ad Statistics
Times Displayed: 1995
Times Visited: 19 Keep biomedical devices ready to go, so care teams can be ready to care for patients. GE HealthCare’s ReadySee™ helps overcome frustrations due to lack of network and device visibility, manual troubleshooting, and downtime.
As the field migrates away from 2-D imaging and toward industrywide adoption of the newer technology, the growth of BT has presented the imaging field with a conundrum. Now that we can find more hard-to-see cancerous lesions and subtle calcifications under 3-D imaging, I and many of my peers are quickly discovering that traditional 2-D imaging is no longer sufficient for re-identifying and targeting those suspicious areas first found with breast tomosynthesis.
As a result, we’re beginning to see tomosynthesis integrated into other areas of breast health, allowing doctors and patients to experience the full spectrum of its benefits. Most recently, with the introduction of BT into image-guided breast biopsies and surgical staging, physicians have been able to use the advanced imaging to quickly pinpoint suspicious lesions or calcifications found during screening.
Beyond imaging: Breast tomosynthesis in biopsies
While the introduction of breast tomosynthesis has been a significant advancement for breast cancer screening, it presented a problem we didn’t know we had. We were detecting more hard-to-find lesions and faint calcifications, yet they could only be seen with 3-D imaging, which created a challenge when it came time to perform a 2-D imaging-guided breast biopsy. It was a frustrating realization of the limits of traditional breast biopsy that unfortunately resulted in a much longer biopsy procedure than necessary, and often translated into more time under compression for the patient, uncertainty for the clinician and inefficiencies for the facility.
Since that time, breast tomosynthesis has made its way into breast biopsy. First, with the integration into upright biopsy and, most recently, prone. While 3-D imaging-guided biopsy in the upright position provided new capabilities to breast biopsy, in most cases, I still opted to biopsy in the prone position, as I prefer the positioning and find patients have a better overall experience without having direct view of the needle. Though, in the cases when upright biopsy is necessary, the added capability of 3-D imaging is beneficial, as we provide breast tomosynthesis screening to the majority of our patients. Given all of this, my facility quickly adopted prone 3-D imaging-guided breast biopsy when it became available because we recognized the shortcomings of the current prone breast biopsy procedure, and we’ve immediately seen a difference since adoption. I am now able to more quickly identify challenging lesions and better target them using the same modality that initially detected the area of concern. The result: my patients can potentially spend less time under compression, reducing overall procedure time and improving their satisfaction. In some more extreme cases, I’ve even been able to biopsy patients who in the past may have required open surgical biopsy, clearly saving the health care system costs, but more importantly, alleviating the patient from the anxiety that comes with any surgical procedure and especially one that could result in a potential breast cancer diagnosis.