by
John R. Fischer, Senior Reporter | January 04, 2018
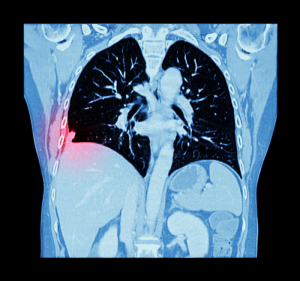
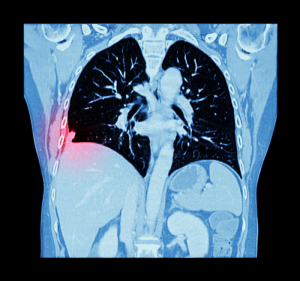
Lung cancer screenings based on
individual risk may save more lives
but be more costly and not ensure
substantial quality-adjusted
-life-years
Lung cancer screenings based on individual risk could potentially save more lives than current recommendations but may be pricey and not offer substantial gains in life-years saved or quality-adjusted-life-years (QALYs).
Those are the findings of two studies published in
Annals of Internal Medicine, with one asserting that individual risk assessment ensures fewer deaths than adherence to current standards while the other claims that such an approach produces fewer QALYs among high-risk individuals and is more costly.
The first, conducted by researchers from the National Cancer Institute (NCI), compared individualized, risk-based eligibility to criteria of the U.S. Preventive Services Task Force (USPSTF), which asserts that individuals between 55 and 80 who currently smoke or have quit in the last 15 years with a 30-pack-year history are eligible for low-dose CT screenings.



Ad Statistics
Times Displayed: 6
Times Visited: 2 Fast-moving cardiac structures have a big impact on imaging. Fujifilm’s SCENARIA View premium performance CT brings solutions to address motion in Coronary CTA while delivering unique dose saving and workflow increasing benefits.
“There is growing consensus in the field that the current USPSTF guidelines may exclude some smokers at high risk of lung cancer who could also benefit from lung cancer screening,” Li C. Cheung, an NCI statistician and one of the coauthors of the first study, told HCB News. “The use of individualized risk calculators and individualized risk-based screening could guard against such exclusion of high risk smokers from screening. Future screening guidelines may well incorporate individualized risk-based screening thresholds for the selection of smokers.”
Using data from the National Health Interview Survey as a basis, the study estimated the effect of eligibility on lung cancer deaths preventable through screening since 2005 and found that the Lung Cancer Risk Assessment Tool could identify high-risk moderate smokers with histories of 20-29 packs per year, and that such an approach could have prevented 5000 more deaths in 2015.
Researchers at Tufts Medical Center conducted the second, evaluating cost-effectiveness of a risk-targeted screening strategy against criteria of the National Lung Screening Trial by estimating the QALYs gained relative to the cost of screening.
Though targeting low-dose CT (LDCT) was found to more likely detect cancer in high-risk patients and avert death over all seven years of the trial, such patients were found to be older with greater smoking exposure, and more likely to have a preexisting diagnosis of chronic obstructive pulmonary disease, giving them a shorter life expectancy and lower quality of life.
Researchers concluded that preventing death in such patients produced fewer QALYs than in patients with lower risk. Furthermore, LDCT screenings of high risk patients was found to lead to more invasive testing, thereby increasing costs.
However, the second study asserts that risk-based identification of people who should undergo screening is empirically superior to current guidelines. It also claims the most pressing concern in lung cancer screening is the fact that people, regardless of their eligibility, are not undergoing screenings, a sentiment echoed by Cheung.
“The biggest challenge facing lung cancer screening in the U.S. today is low uptake,” he told HCB News. “The specific strategies for the selection of smokers notwithstanding, uptake of lung cancer screening in the U.S. population has been low, and only around 4 percent of eligible smokers have undergone screening. Physicians and other health care professionals should encourage all eligible smokers to undergo lung cancer screening.”
Researchers from Tufts did not respond for comment.